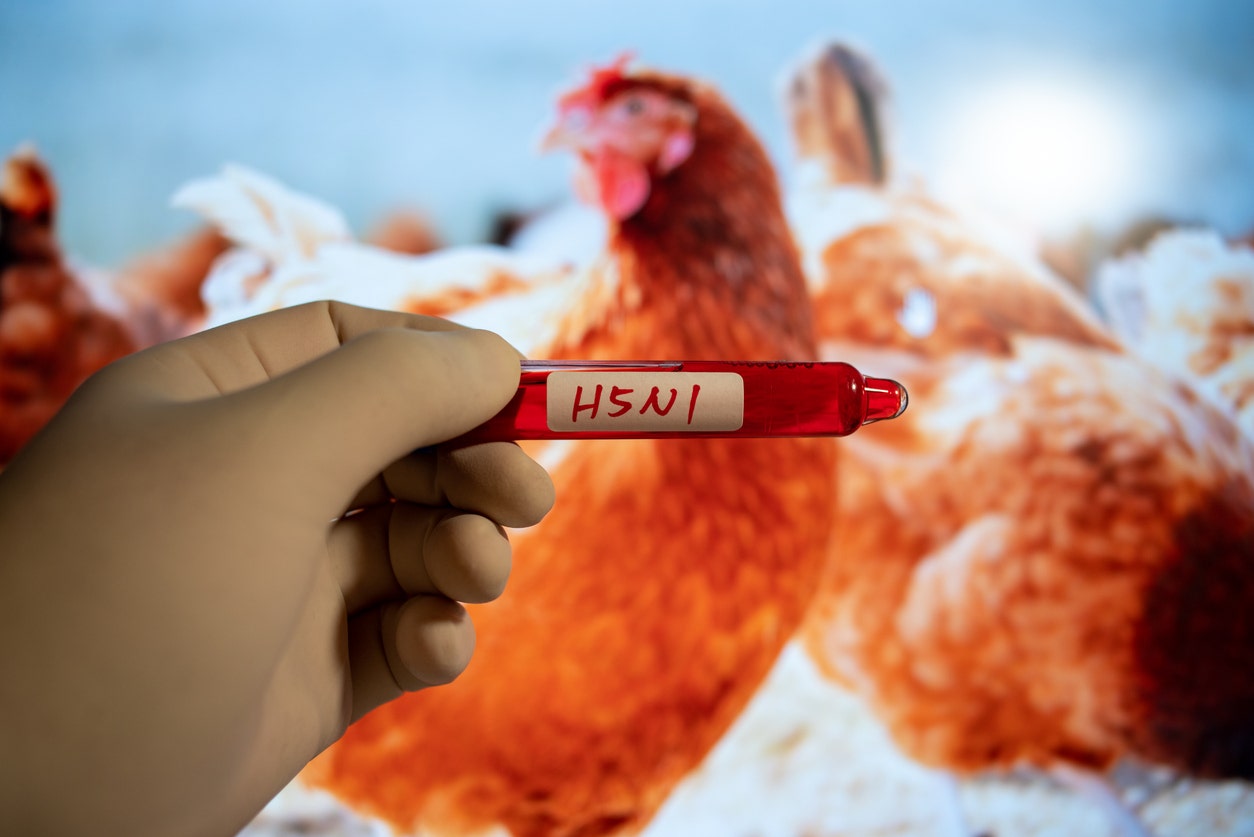
First Case of Human Bird Flu in the U.S. Without Animal Contact
Brace yourselves, folks! A Missouri patient has become the talk of the town by contracting the bird flu without so much as a casual stroll past a chicken coop. Yes, you heard that right. Not a single feathered friend in sight.


The Centers for Disease Control and Prevention (CDC) confirmed this quirky and somewhat concerning case of avian influenza A (H5) on a recent Friday. Our feathery-less patient, who was apparently already dealing with other health issues, was successfully treated and is now back to binge-watching their favorite shows.
Oh, and did we mention this marks the 14th person in the U.S. to catch the bird flu this year? But unlike the other 13 unlucky souls who had been hanging out with dairy cows or poultry, this one didn’t!

According to Dr. Benjamin Anderson from the University of Florida, it’s pretty unsettling to test positive for H5 without the usual animal exposure. The good doctor pointed out we’re still clueless about the details, asking the million-dollar question: “Indirect exposure, maybe?”
And to spice things up, Dr. Edward Liu from Hackensack Meridian Jersey Shore University Medical Center threw his hat in the ring, raising concerns about human-to-human spread. If that happens, forget animals—humans will be the new vectors!

Experts believe the virus might adapt to replicate more efficiently in humans, spreading through those delightful respiratory droplets and secretions. Think coughing and sneezing—our collective worst nightmare from 2020.
Liu also emphasized our current testing for bird flu isn’t exactly a blockbuster hit. If our run-of-the-mill influenza A cases spike, some might actually be avian influenza in disguise. Oh joy, an iceberg of flu cases, just what we needed.

Risk Factors and Next Steps
The risk factor du jour? The possibility of the bird flu mutating to spread from one human to another. Let’s give a big hand to nature for always keeping us on our toes.
Dr. Anderson informed us that influenza viruses can evolve through both small mutations and rapid recombination, like remixing viral genes into new, possibly scarier viruses. We should especially watch those with dairy cow and poultry exposure, where these “spillovers” have occurred.
So far, infections in dairy cow strains have mostly been mild, but viruses are like cat videos—they always evolve. Monitoring the circulation of these viruses is key.
For those keeping score, avian influenza isn’t included in our seasonal flu vaccines, though the shot might still offer some shield. Current antivirals, like Tamiflu, are fortunately still in the game to treat bird flu.

The high-risk groups include older adults, young children, immunocompromised folks, and those with chronic ailments. Pretty much, if you’re not chomping kale and running marathons, you might want to stay updated.
In the realm of reality checks, Dr. Marc Siegel noted that while we haven’t seen human-to-human transmission yet, it’s important to stay vigilant. If that happens, it’s a game changer.
The CDC reassured the public that the bird flu risk remains low, but they’re keeping a close eye on this situation, with investigations continuing both in the laboratory and on the ground.
Stay tuned, stay educated, and keep those hands washed. After all, you never know who’s catching more than just a case of the gigs at your next gathering.